Abstract
Inflatable penile prosthesis (IPP) is an effective treatment for erectile dysfunction in patients’ refractory to oral or injectable treatment. While the rate of infection has decreased over the past decade, it is still the most feared complication of IPP placement. Here, we assemble possible patient and surgical factors attributing to the risk of infection. Studies have been gathered addressing each of these factors, and an Oxford Level of Evidence is assigned to each recommendation based on strength of the study. The goal of this review is to inform surgeons of possible risks in order to further reduce the risk of infection and thus increase success of IPP placement.
Similar content being viewed by others
References
Lindeborg L et al. Satisfaction and complications with the Titan(R) one-touch release penile implant. Scand J Urol. 2014;48(1):105–9.
Bettocchi C et al. Patient and partner satisfaction after AMS inflatable penile prosthesis implant. J Sex Med. 2010;7(1 Pt 1):304–9.
Carson CC, Mulcahy JJ, Govier FE. Efficacy, safety and patient satisfaction outcomes of the AMS 700CX inflatable penile prosthesis: results of a long-term multicenter study. AMS 700CX Study Group. J Urol. 2000;164(2):376–80.
Henry GD, Wilson SK. Updates in inflatable penile prostheses. Urol Clin North Am. 2007;34(4):535–47. vi.
Montague DK. Periprosthetic infections. J Urol. 1987;138(1):68–9.
Chlebicki MP et al. Preoperative chlorhexidine shower or bath for prevention of surgical site infection: a meta-analysis. Am J Infect Control. 2013;41(2):167–73.
Webster J, Osborne S. Preoperative bathing or showering with skin antiseptics to prevent surgical site infection. Cochrane Database Syst Rev. 2012;9:Cd004985.
Darouiche RO et al. North American consensus document on infection of penile prostheses. Urology. 2013;82(4):937–42.
Turan A et al. Smoking and perioperative outcomes. Anesthesiology. 2011;114(4):837–46.
Sorensen LT. Wound healing and infection in surgery. The clinical impact of smoking and smoking cessation: a systematic review and meta-analysis. Arch Surg. 2012;147(4):373–83.
Kigera JW et al. Is there an increased risk of post-operative surgical site infection after orthopaedic surgery in HIV patients? A systematic review and meta-analysis. PLoS One. 2012;7(8):e42254.
Silverstein A, et al. Nasal carriage of Staphylococcus aureus as a potential risk factor for infection after penile prosthesis placement. Int J Impot Res. 2002;14(S61).
Berthelot P et al. Is nasal carriage of Staphylococcus aureus the main acquisition pathway for surgical-site infection in orthopaedic surgery? Eur J Clin Microbiol Infect Dis. 2010;29(4):373–82.
Bode LGM et al. Preventing surgical-site infections in nasal carriers of Staphylococcus aureus. N Engl J Med. 2010;362(1):9–17.
Henry GD et al. Penile prosthesis cultures during revision surgery: a multicenter study. J Urol. 2004;172(1):153–6.
Jarow JP. Risk factors for penile prosthetic infection. J Urol. 1996;156(2 Pt 1):402–4.
Wilson SK, Delk 2nd JR. Inflatable penile implant infection: predisposing factors and treatment suggestions. J Urol. 1995;153(3 Pt 1):659–61.
Wilson SK et al. Infection reduction using antibiotic-coated inflatable penile prosthesis. Urology. 2007;70(2):337–40.
Thomalla JV et al. Infectious complications of penile prosthetic implants. J Urol. 1987;138(1):65–7.
McManus LM et al. Agonist-dependent failure of neutrophil function in diabetes correlates with extent of hyperglycemia. J Leukoc Biol. 2001;70(3):395–404.
Barbul AED. In: Brunicardi ADF, Billiar T, Dunn D, Hunter J, Mathews J, Pollock R, editors. Wound Healing, in Schwartz's Principles of Surgery. Chicago: McGraw Hill Medical; 2010. p. 209–33.
Mulcahy JJ, Carson Iii CC. Long-term infection rates in diabetic patients implanted with antibiotic-impregnated versus nonimpregnated inflatable penile prostheses: 7-year outcomes. Eur Urol. 2011;60(1):167–72.
Garber BB, Marcus SM. Does surgical approach affect the incidence of inflatable penile prosthesis infection? Urology. 1998;52(2):291–3.
Wilson SK et al. Quantifying risk of penile prosthesis infection with elevated glycosylated hemoglobin. J Urol. 1998;159(5):1537–9. discussion 1539–40.
Bishop JR et al. Use of glycosylated hemoglobin to identify diabetics at high risk for penile periprosthetic infections. J Urol. 1992;147(2):386–8.
Goldstein I et al. Radiation-associated impotence. a clinical study of its mechanism. JAMA. 1984;251(7):903–10.
Dubocq FM et al. Outcome analysis of penile implant surgery after external beam radiation for prostate cancer. J Urol. 1997;158(5):1787–90.
Biering-Sorensen F, Sonksen J. Sexual function in spinal cord lesioned men. Spinal Cord. 2001;39(9):455–70.
Collins KP, Hackler RH. Complications of penile prostheses in the spinal cord injury population. J Urol. 1988;140(5):984–5.
Radomski SB, Herschorn S. Risk factors associated with penile prosthesis infection. J Urol. 1992;147(2):383–5.
Tobian AA, Gray RH, Quinn TC. Male circumcision for the prevention of acquisition and transmission of sexually transmitted infections: the case for neonatal circumcision. Arch Pediatr Adolesc Med. 2010;164(1):78–84.
Sidi AA et al. Penile prosthesis surgery in the treatment of impotence in the immunosuppressed man. J Urol. 1987;137(4):681–2.
Ginaldi L et al. The immune system in the elderly: II. Specific cellular immunity. Immunol Res. 1999;20(2):109–15.
Chung E et al. Clinical outcomes and patient satisfaction rates among elderly male aged >/=75 years with inflatable penile prosthesis implant for medically refractory erectile dysfunction. World J Urol. 2014;32(1):173–7.
Gonzalez Chiappe S, et al. Use of clean intermittent self-catheterization in France: A survey of patient and GP perspectives. Neurourol Urodyn. 2015.
Edokpolo LU, Stavris KB, Foster HE. Intermittent catheterization and recurrent urinary tract infection in spinal cord injury. Top Spinal Cord Inj Rehabil. 2012;18(2):187–92.
Diokno AC, Sonda LP. Compatibility of genitourinary prostheses and intermittent self-catheterization. J Urol. 1981;125(5):659–60.
Tanner J, Norrie P, Melen K. Preoperative hair removal to reduce surgical site infection. Cochrane Database Syst Rev. 2011(11):Cd004122.
Darouiche RO et al. Chlorhexidine-alcohol versus povidone-iodine for surgical-site antisepsis. N Engl J Med. 2010;362(1):18–26.
Paocharoen V, Mingmalairak C, Apisarnthanarak A. Comparison of surgical wound infection after preoperative skin preparation with 4% chlorhexidine [correction of chlohexidine] and povidone iodine: a prospective randomized trial. J Med Assoc Thail. 2009;92(7):898–902.
Parienti JJ et al. Hand-rubbing with an aqueous alcoholic solution vs traditional surgical hand-scrubbing and 30-day surgical site infection rates: a randomized equivalence study. JAMA. 2002;288(6):722–7.
Weber WP et al. Surgical hand antisepsis with alcohol-based hand rub: comparison of effectiveness after 1.5 and 3 minutes of application. Infect Control Hosp Epidemiol. 2009;30(5):420–6.
Mandava SH et al. Infection retardant coated inflatable penile prostheses decrease the incidence of infection: a systematic review and meta-analysis. J Urol. 2012;188(5):1855–60.
Yerdel MA et al. Effect of single-dose prophylactic ampicillin and sulbactam on wound infection after tension-free inguinal hernia repair with polypropylene mesh: the randomized, double-blind, prospective trial. Ann Surg. 2001;233(1):26–33.
Boxma H et al. Randomised controlled trial of single-dose antibiotic prophylaxis in surgical treatment of closed fractures: the Dutch Trauma Trial. Lancet. 1996;347(9009):1133–7.
Wolf Jr JS et al. Best practice policy statement on urologic surgery antimicrobial prophylaxis. J Urol. 2008;179(4):1379–90.
Sadeghi-Nejad H et al. Multi-institutional outcome study on the efficacy of closed-suction drainage of the scrotum in three-piece inflatable penile prosthesis surgery. Int J Impot Res. 2005;17(6):535–8.
Eid JF et al. Coated implants and "no touch" surgical technique decreases risk of infection in inflatable penile prosthesis implantation to 0.46%. Urology. 2012;79(6):1310–5.
Cahill PJ et al. The effect of surgeon experience on outcomes of surgery for adolescent idiopathic scoliosis. J Bone Joint Surg Am. 2014;96(16):1333–9.
Sgroi MD et al. Experience matters more than specialty for carotid stenting outcomes. J Vasc Surg. 2015;61(4):933–8.
LaPar DJ et al. Mitral valve repair rates correlate with surgeon and institutional experience. J Thorac Cardiovasc Surg. 2014;148(3):995–1003. discussion 1003–4.
Henry GD et al. Centers of excellence concept and penile prostheses: an outcome analysis. J Urol. 2009;181(3):1264–8.
Graf K et al. Decrease of deep sternal surgical site infection rates after cardiac surgery by a comprehensive infection control program. Interact Cardiovasc Thorac Surg. 2009;9(2):282–6.
Stulberg JJ et al. Adherence to surgical care improvement project measures and the association with postoperative infections. JAMA. 2010;303(24):2479–85.
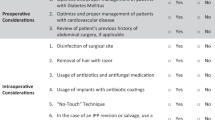
Katz BF et al. Use of a preoperative checklist reduces risk of penile prosthesis infection. J Urol. 2014;192(1):130–5.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Bradley Holland declares no potential conflicts of interest.
Tobias Kohler reports grants and personal fees from AMS and Coloplast.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Men’s Health
Rights and permissions
About this article
Cite this article
Holland, B., Kohler, T. Minimizing Penile Implant Infection: A Literature Review of Patient and Surgical Factors. Curr Urol Rep 16, 81 (2015). https://doi.org/10.1007/s11934-015-0554-2
Published:
DOI: https://doi.org/10.1007/s11934-015-0554-2